Health
Best Lubricant for Menopause: Review 2020
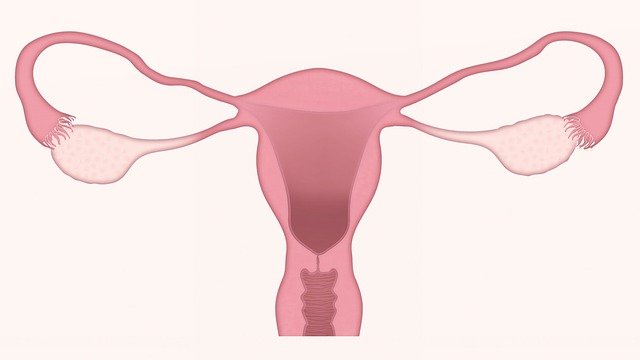
With the onset of the menopause in the female body, the reproductive function gradually fades, and complex hormonal changes occur due to a decrease in the production of sex hormones: estrogen and progesterone. This, in turn, results in vaginal dryness and discomfort while having sex. Using the best lubricant for menopause dryness, a woman is capable to deal with the problem that has arisen without giving up her intimate life.
Causes of Dry Mucous Membranes With Menopause
The epithelium of the vagina and cervix produces a special lubricant, which is necessary to ensure a comfortable state in the intimate zone. Its presence in sufficient quantities prevents the appearance of dryness in the vagina and creates protection against pathogens. The processes of production and release of lube are affected by the level of estrogen. The best natural lubricant for menopause dryness is designed to solve the issue.
In the climacteric, the hormonal function of the ovaries gradually fades, they reduce the production of sex hormones, and eventually completely stop. Therefore, the main reason that lube is produced in the climacteric in smaller quantities is a decrease in estrogen levels. The menopausal dryness of the vagina does not disappear with time but only worsens. That is why the usage of the best lubricant for menopause dryness is literally inevitable.
Menopause vaginal dryness may provoke the following conditions:
- mucous membranes thin and atrophy;
- microcracks appear;
- candidiasis or thrush develops;
- the risk of contracting other fungal diseases increases;
- inflammatory processes appear.
A decrease in the amount of natural lube in the vagina leads to a change in the level of acidity of the medium and causes itching and sometimes burning. In this case, the best lubricant for menopause will save the situation.
Types of the Best Sexual Lubricant for Menopause
Lubricants are designed to improve the quality of intimate relationships. They envelop the mucous membrane and facilitate gliding during sexual contact with menopause, and also protect its epithelium from microtrauma.
There are 3 types of lubes:
- Water-based. It is very popular in menopausal women. It has a number of advantages: the best personal lubricant for menopause on a water base has a rather pleasant consistency, quickly penetrates the epithelial tissue, does not leave stains on bedding and clothes, and does not enter into chemical reactions with latex, and therefore can be used with condoms. The best lubricant for intercourse after menopause also does not cause irritation and can be used for intimacy by women prone to allergic reactions. Another positive point is the low cost. Its significant drawback is quick drying. During intimacy, you have to apply the product several times, which might reduce the quality of sex.
- The best lubricant for sex after menopause based on silicone. This substance greatly enhances gliding during sexual contact. The tool can be used in conjunction with contraceptives. The action lasts a long time. It has 2 significant drawbacks: leaves stains on linen and is difficult to rinse off.
- With the addition of mineral oils that do not harm the organs of the reproductive system of women. The product has a rather dense and viscous consistency. It is not recommended to combine it with the use of condoms and intimate toys due to the possibility of unwanted reactions. The disadvantages include the appearance of stains on the bedding.
Important! Lubricants, regardless of type, should be bought only at pharmacies and sex shops that have a quality certificate on them.
How to Choose the Best Personal Lubricant for Menopause
Doctors made general recommendations on how to choose the best lubricant for menopause:
- Preference should be given to means with lactic acid, which maintains a normal pH level for the intimate zone and has the ability to restore the vaginal microflora.
- Avoid products containing sugar, which leads to a violation of the microflora in the vagina.
- It is advisable to choose lubes without parabens, dyes, and fragrances that can cause itching and other irritations of the mucosa.
- The product may include extracts of natural plants: aloe vera, chamomile, calendula, etc.
- The presence of panthenol, which moisturizes the mucous membranes, as well as vitamin E, sea buckthorn oil, and other oils, is acceptable.
- The best lubricant for menopause dryness may include an antibacterial component.
Rules for the Use of Intimate Lubricants
Lubricants are applied after a hygiene procedure using a liquid for intimate places. A small amount of gel or cream is applied to the carefully wiped palm of the leading hand and is distributed evenly over the entire surface in the area of the vestibule and the vaginal wall.
Using the applicator, which is in the same package with the lubricant, the agent in the amount indicated in the instructions is injected into the vagina.
A gel-like lubricant is also applied over the entire surface of the partner’s penis, and when using a condom on top of it. After intercourse, the best lubricant for menopause is washed off with warm water.
Health
Snack Smarter: The Rise of Low-Calorie Almond Butter for Active Lifestyles

The snack aisle is shifting. For those who balance a busy life with a commitment to health and fitness, the rise of low-calorie almond butter offers a new way to snack smarter. American Dream Nut Butter is at the center of this change, blending clean ingredients with dessert-inspired flavors and added protein to create almond butter that is both nutritious and enjoyable.
Why Almond Nut Butter Is Key to Clean Eating
As consumers become more mindful of their food choices, the spotlight is increasingly on nutrient-dense snacks that provide sustained energy without excess calories. Almond butter, especially in low-calorie varieties, meets this demand by offering a rich source of healthy fats, fiber, and protein in a compact form. Compared to traditional spreads, such as peanut butter, almond butter often provides a smoother, lighter alternative with a different nutritional profile.
For those who track macros or embrace meal prepping, almond nut butter fits neatly into their plans. Its balance of fats and protein supports satiety, helping to keep hunger at bay between meals or during workouts. American Dream Nut Butter elevates this concept with high-protein options that blend the wholesome qualities of almonds with a subtle sweetness inspired by classic desserts.
How Much Protein is in Low Calorie Almond Butter for High Performance?
One common question around almond butter is: how much protein does almond butter contain? While natural almond butter provides a moderate protein boost, American Dream Nut Butter takes it a step further by creating blends that enhance protein content without relying on artificial sweeteners or fillers. This approach suits those seeking fuel for recovery or sustained energy throughout their day.
These protein-enhanced almond butters can work as a pre-workout snack, a post-exercise treat, or simply as a midday pick-me-up that aligns with a health-conscious lifestyle. The brand’s small-batch production method ensures each jar maintains a fresh, creamy texture that spreads easily or drizzles beautifully over everything from oatmeal to fruit.
Buy Almond Butter: Unique Flavors from American Dream

American Dream Nut Butter distinguishes itself with unique flavor profiles, such as Cinnamon Toasties and Cookie Batter. These offerings embrace the idea that healthful snacks can still delight the palate, using clean, natural ingredients to create indulgent taste experiences without sugar bombs or artificial additives. Each batch is hand-whipped in-house, reflecting the brand’s commitment to quality and care.
Their dedication to natural flavors and nutrient density allows consumers to enjoy a dessert-inspired snack while keeping their wellness goals intact. Whether you’re looking to buy almond butter that tastes like a treat or are curious where you can find almond butter crafted with both nutrition and flavor in mind, American Dream Nut Butter offers an accessible option.
Almond Nut Butter: Fuel for Athletes and Busy Parents
Almond butter’s versatility makes it appealing for a wide range of active lifestyles. For athletes, it provides a balanced blend of nutrients that supports energy and recovery without unwanted additives. For busy parents or professionals juggling multiple demands, it’s a convenient, clean snack that fits into hectic schedules without compromise.
The brand’s YouTube channel offers video insight into how these nut butters are crafted, revealing the hands-on process that ensures quality in every jar. By choosing American Dream Nut Butter, consumers support a product that embodies family values and a personal story of overcoming dietary challenges to create wholesome alternatives that everyone can enjoy.
Where Can You Find the Best Almond Butter & More? The Future Is Here
The growing interest in low-calorie nut butter reflects a broader shift in how people approach snacking—valuing nutrition, flavor, and mindful eating in equal measure. American Dream Nut Butter’s approach, which combines protein-rich formulas with all-natural ingredients and enticing flavors, shows how almond butter, peanut butter, and cashew butter can evolve from a niche health food into a daily staple for those who want to snack smarter.
For more on the evolving nut butter market and how it aligns with fitness trends, check out this feature on the rise of healthy high-protein nut butter. To explore American Dream Nut Butter’s full collection and shop their almond butter selections, visit their website.
American Dream Nut Butter invites you to experience healthy nut butters that strikes a balance between enjoyment and mindful nutrition—perfect fuel for active days and wellness routines alike.
*Images sourced from American Dream Nut Butter
-

 Tech4 years ago
Tech4 years agoEffuel Reviews (2021) – Effuel ECO OBD2 Saves Fuel, and Reduce Gas Cost? Effuel Customer Reviews
-

 Tech6 years ago
Tech6 years agoBosch Power Tools India Launches ‘Cordless Matlab Bosch’ Campaign to Demonstrate the Power of Cordless
-

 Lifestyle6 years ago
Lifestyle6 years agoCatholic Cases App brings Church’s Moral Teachings to Androids and iPhones
-

 Lifestyle4 years ago
Lifestyle4 years agoEast Side Hype x Billionaire Boys Club. Hottest New Streetwear Releases in Utah.
-

 Tech7 years ago
Tech7 years agoCloud Buyers & Investors to Profit in the Future
-

 Lifestyle5 years ago
Lifestyle5 years agoThe Midas of Cosmetic Dermatology: Dr. Simon Ourian
-

 Health6 years ago
Health6 years agoCBDistillery Review: Is it a scam?
-

 Entertainment6 years ago
Entertainment6 years agoAvengers Endgame now Available on 123Movies for Download & Streaming for Free
